





Imagine your body's cells are like a house with a locked door, and glucose (sugar from food) is the essential energy needed to power everything inside. Insulin is the key that unlocks that door, allowing glucose to enter the cells from the bloodstream.
In a healthy individual, the pancreas releases insulin when blood glucose levels rise after a meal. Insulin acts on the cell membrane, signaling it to open up specific "channels" (called glucose transporters) so glucose can be efficiently taken in and used for energy or stored for later [1, 2].
In people with diabetes, this system breaks down in one of two main ways:
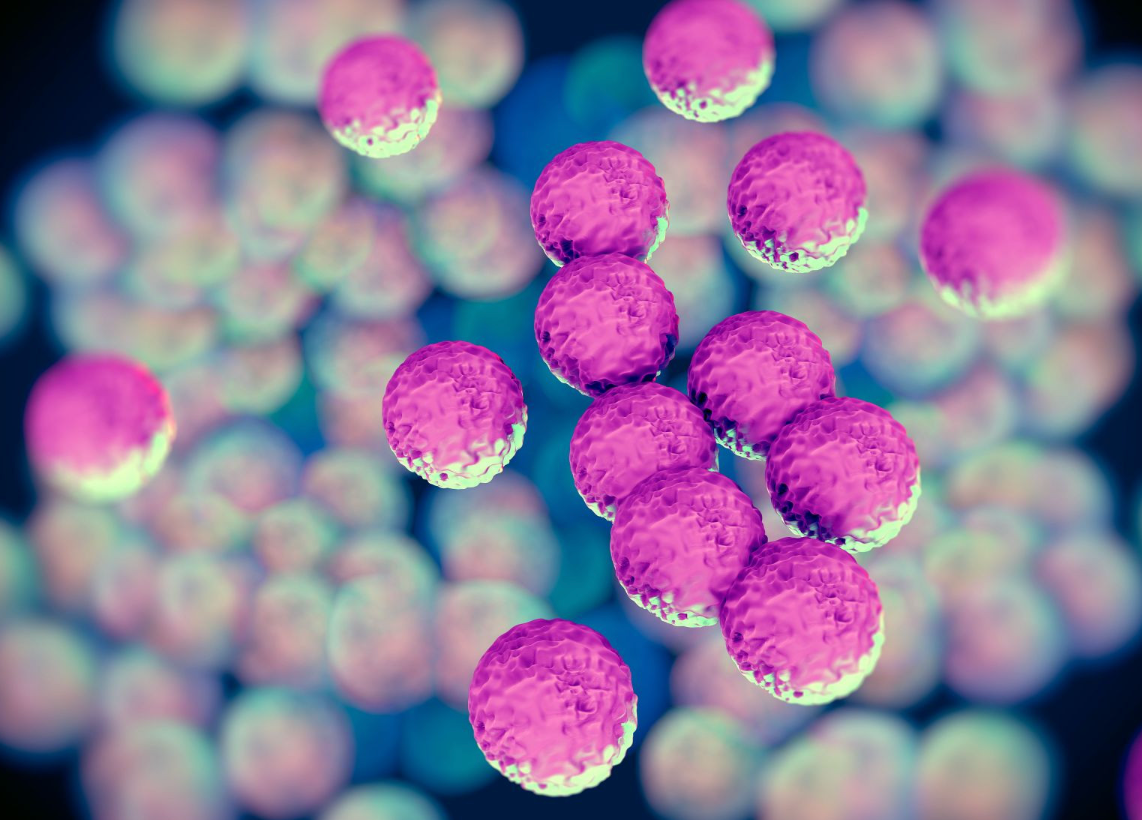
Type 1 Diabetes: The Missing Key
In type 1 diabetes, the immune system mistakenly attacks and destroys the insulin-producing cells in the pancreas [2, 3]. As a result, the body produces very little or no insulin.
The Problem: The key is missing.
The Effect: Without insulin, the cell doors remain locked. Glucose cannot enter the cells and builds up in the bloodstream [2]. The cells, starving for energy despite being surrounded by fuel, send signals of hunger, while the blood sugar levels remain dangerously high.
Type 2 Diabetes: The Broken Lock or Wrong Key
Type 2 diabetes is the most common form, and it's characterized by insulin resistance, where the body's cells don't respond properly to insulin [2, 3].
The Problem: The lock is broken or jammed.
The Effect: The pancreas tries to compensate by producing more and more insulin, but the cells ignore the signal [2]. It's like trying to use the right key on a faulty lock—it just won't turn. Eventually, the pancreas can't keep up with the demand, insulin production drops, and glucose accumulates in the blood [2].
The Consequences of Starving Cells
When cells can't access glucose, they look for alternative energy sources. They start breaking down fat and muscle, leading to weight loss and fatigue [2]. In the case of type 1 diabetes, this can produce toxic byproducts called ketones, leading to a serious condition called diabetic ketoacidosis (DKA) [2].
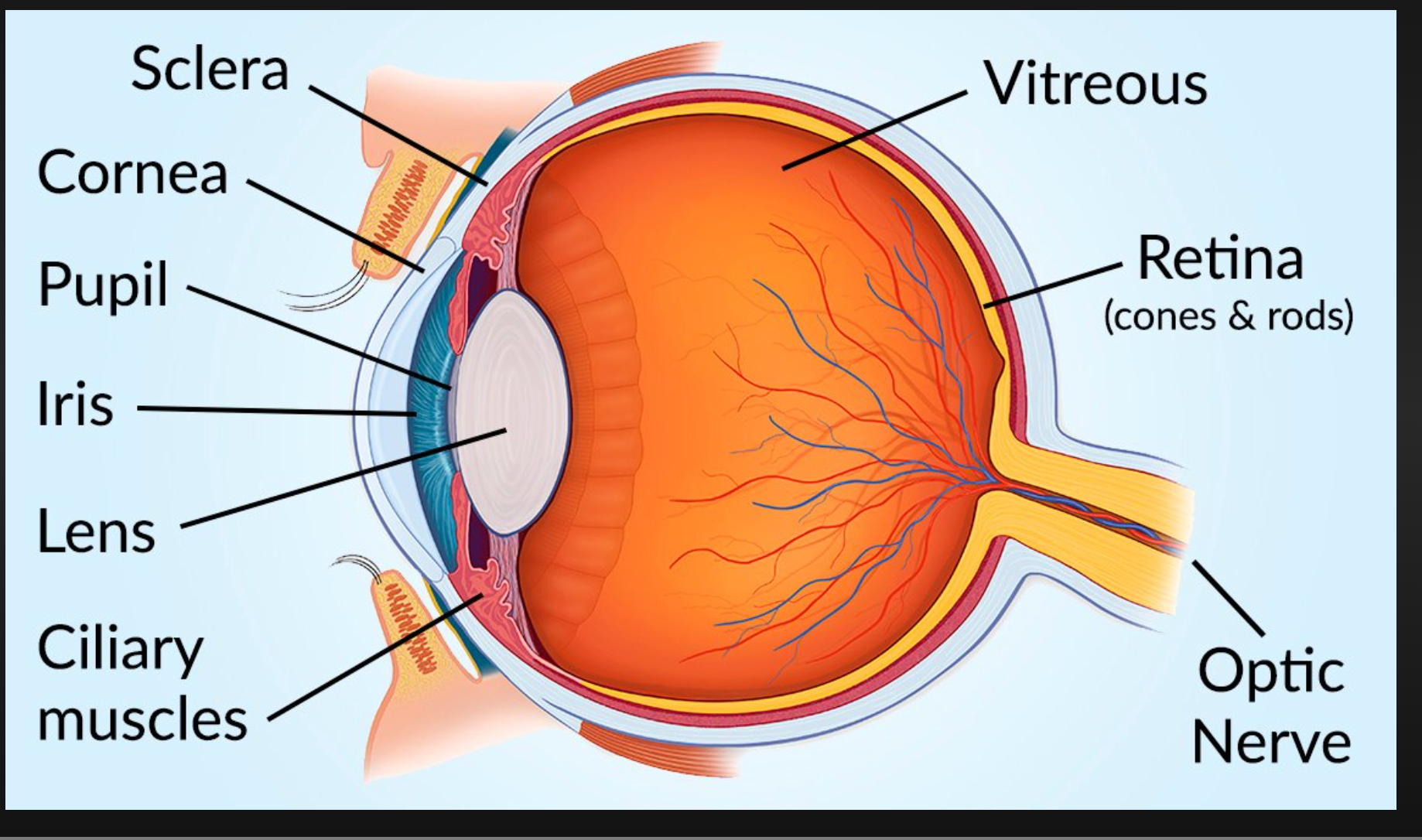
Over time, this excess glucose circulating in the blood causes damage to blood vessels, nerves, kidneys, and eyes, which are the long-term complications associated with diabetes [2].
Managing the Mechanism
Understanding this cellular malfunction is key to managing diabetes. Treatments focus on:
Type 1: Replacing the missing key through insulin injections or pumps [2].
Type 2: Improving the lock mechanism through lifestyle changes (diet and exercise) and medications that enhance insulin sensitivity or help the body manage blood sugar levels [2, 3].
By managing blood glucose and helping the cells get the fuel they need, individuals with diabetes can live healthy and active lives.
