When Calcium Crystals Attack: How Hydroxyapatite Deposition Disease (HADD) Steals Your Mobility—and How to Fight Back!
Have you ever woken up with searing pain in your shoulder, hip, or knee and wondered how a seemingly healthy joint could suddenly betray you? You might be surprised to learn that tiny calcium crystals—specifically hydroxyapatite—can build up in the tendons and soft tissues around your joint and cause intense, sometimes debilitating pain.
This condition is called Hydroxyapatite Deposition Disease (HADD), and it’s more common than many people realize.
Why HADD Matters
HADD is often mistaken for bursitis, tendonitis, or rotator cuff injuries. Because its onset can be sudden and dramatic, many people rush to imaging centers or emergency rooms for answers. Understanding HADD helps patients get the right diagnosis and faster relief—without unnecessary procedures.
What is Hydroxyapatite Deposition Disease?
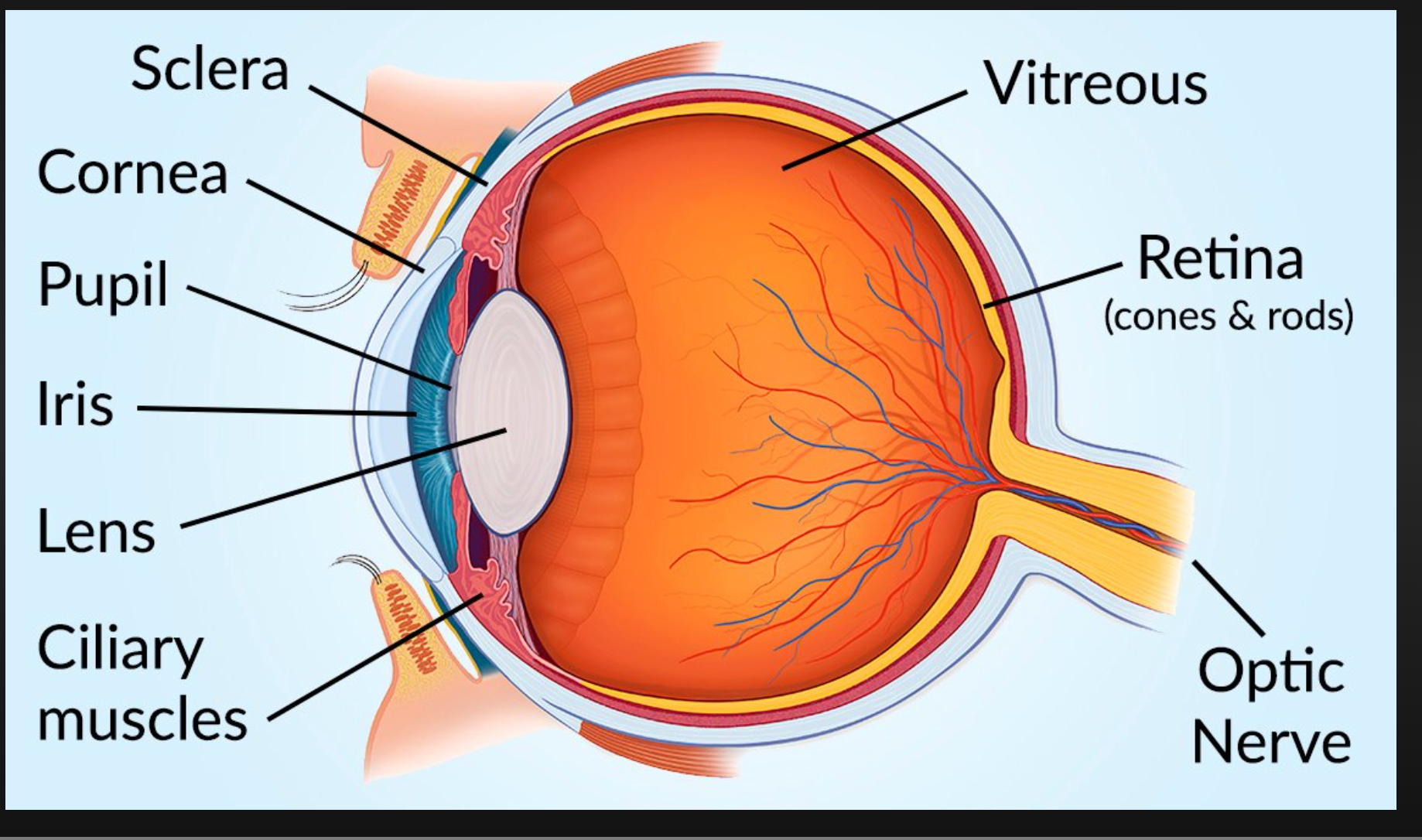
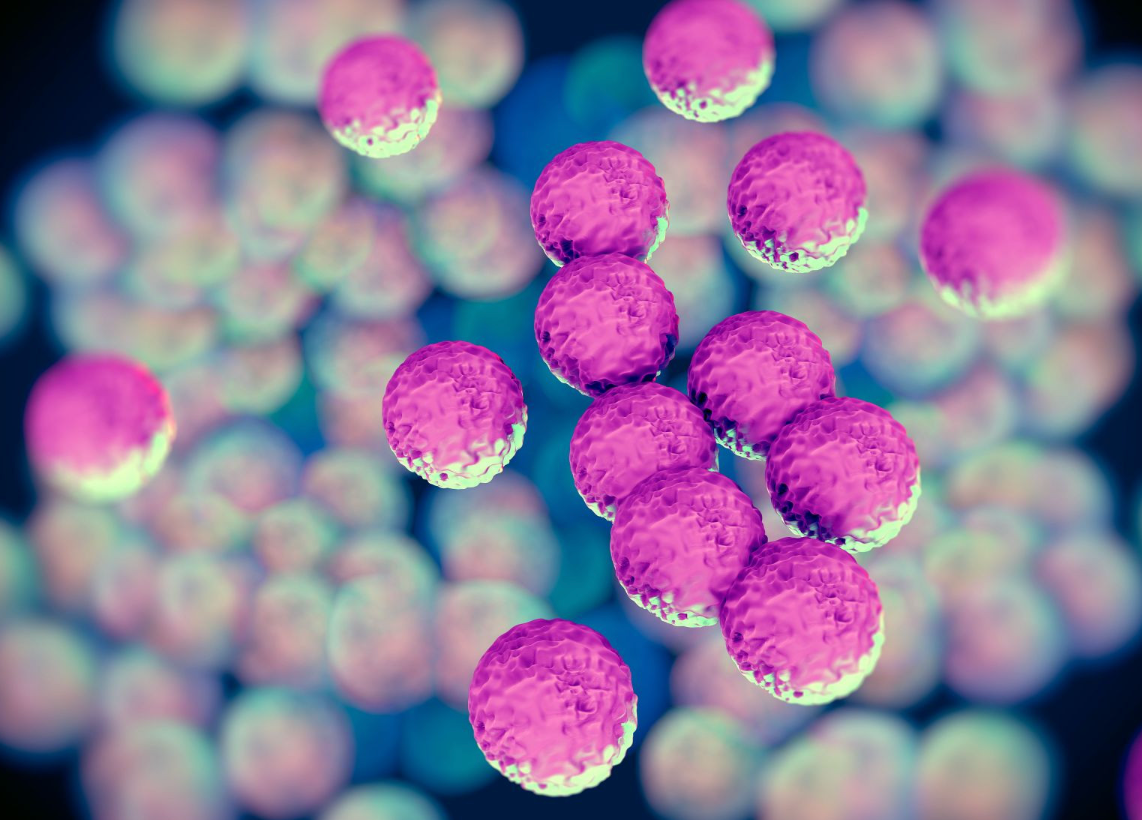
HADD occurs when hydroxyapatite crystals (a form of calcium phosphate) deposit in tendons, bursae, or other soft tissues near joints. The shoulder is the most commonly affected area, particularly the rotator cuff tendons, but HADD can also affect the hip, wrist, elbow, knee, and other sites. Deposits can trigger an acute inflammatory response, producing severe pain, swelling, and restricted movement.
Common symptoms
Sudden, intense joint pain—often waking people at night.
Local swelling and warmth.
Severely limited range of motion (e.g., unable to lift your arm).
Pain that may come in waves: a painful acute phase followed by weeks of gradual improvement.
Symptoms can sometimes mimic an infection, so a medical evaluation is important.
Who gets HADD?
HADD most often affects adults between 30 and 60 years old, though it can occur at any age. There’s no single known cause, but factors like repetitive microtrauma, metabolic conditions, and local tissue degeneration may contribute. Many patients have no obvious risk factor.
How it’s diagnosed?
Clinical history and physical exam: doctors note the suddenness and pattern of pain.
X-rays: can reveal calcific deposits near the joint.
Ultrasound: Excellent for identifying and localizing deposits, as well as guiding injections or procedures.
MRI: used if other conditions need to be ruled out.
Aspiration/analysis: rarely required; usually, imaging is enough.
Treatment options that relieve pain and restore function?
The good news is that many people recover well with conservative care.
Options include:
Rest, ice, and short-term use of NSAIDs for pain control.
Corticosteroid injections into the bursa or tendon to reduce inflammation (often ultrasound-guided for accuracy)
Physical therapy to restore the range of motion and strengthen the surrounding muscles
Ultrasound-guided needle lavage (barbotage): a procedure that breaks up and flushes out the calcium deposit, can provide rapid relief.
Extracorporeal shock wave therapy (ESWT): a noninvasive option used in some centers to break up deposits.
Arthroscopic surgery: reserved for persistent cases that fail conservative measures.
Prognosis and recurrence
Many acute HADD episodes are self-limited over weeks to months, especially with targeted therapy. However, deposits can recur or persist; timely treatment improves outcomes and reduces the risk of long-term stiffness.
When to seek urgent care?
If severe pain is accompanied by fever, spreading redness, or rapidly worsening symptoms, seek immediate medical attention—these signs could indicate infection or another serious condition.
Hydroxyapatite Deposition Disease can be frightening when it strikes, but with the right diagnosis and targeted treatment, many people regain full function quickly. If you’ve had sudden, severe joint pain—or repeated “mysterious” flareups—don’t shrug it off. Get informed, check your symptoms, and connect with a provider who knows how to treat HADD effectively.